Abdominal pain, a common ailment, can stem from a myriad of sources, ranging from simple indigestion to serious conditions requiring immediate medical attention. Understanding the location, character, and associated symptoms of abdominal pain is crucial for accurate diagnosis and appropriate management. This guide explores ten common types of abdominal pain, providing insights into their causes, symptoms, and diagnostic approaches to empower you with the knowledge to seek timely and effective care.
Navigating the complexities of abdominal pain requires a systematic approach. We will delve into the anatomy of the abdomen, differentiating between visceral and somatic pain, and examining various diagnostic tools, including physical examinations, blood tests, and imaging studies. By understanding the distinct characteristics of pain associated with different organs and systems, we can effectively narrow down potential causes and guide appropriate diagnostic strategies. This guide will equip you with a clearer understanding of how to interpret abdominal pain and when to seek professional medical assistance.
Understanding Abdominal Pain Locations and Characteristics
Abdominal pain is a common complaint, and its accurate diagnosis relies heavily on understanding the location and characteristics of the pain. Pinpointing the source of the pain requires considering both the anatomical location within the abdomen and the specific qualities of the pain itself. This understanding allows for a more focused approach to determining the underlying cause.
Abdominal Quadrants and Associated Organs
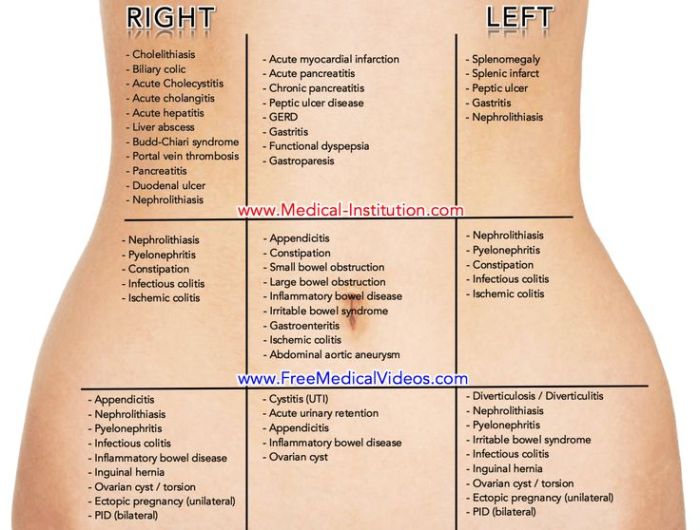
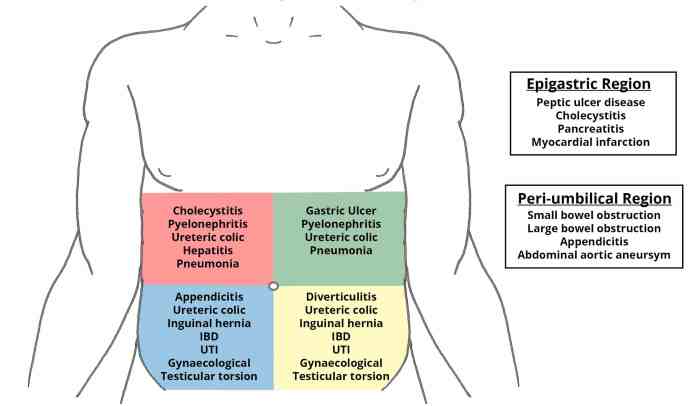
The abdomen is divided into four quadrants: right upper quadrant (RUQ), left upper quadrant (LUQ), right lower quadrant (RLQ), and left lower quadrant (LLQ). Each quadrant contains specific organs, and pain originating from these organs often presents in a characteristic way. Knowing the organ location helps narrow down potential diagnoses.
| Quadrant | Associated Organs | Common Pain Types | Possible Causes of Pain |
|---|---|---|---|
| Right Upper Quadrant (RUQ) | Liver, gallbladder, part of the small intestine, right kidney | Sharp, stabbing, dull, aching | Gallstones, hepatitis, liver abscess, kidney infection |
| Left Upper Quadrant (LUQ) | Stomach, spleen, pancreas, part of the small intestine, left kidney | Burning, cramping, sharp, dull | Gastritis, pancreatitis, splenic rupture, kidney stones |
| Right Lower Quadrant (RLQ) | Appendix, right ovary (in women), right ureter | Sharp, cramping, localized | Appendicitis, ovarian cysts, kidney stones, pelvic inflammatory disease |
| Left Lower Quadrant (LLQ) | Part of the small intestine, left ovary (in women), sigmoid colon | Cramping, dull, aching | Diverticulitis, ovarian cysts, irritable bowel syndrome |
Characteristics of Abdominal Pain
The nature of abdominal pain – its quality, intensity, and timing – provides valuable clues to its origin. Different pain characteristics often point to different underlying conditions.
Sharp pain is often associated with sudden, serious conditions like appendicitis, kidney stones, or a perforated ulcer. Imagine the sudden, intense pain felt when a gallstone blocks the cystic duct, causing a sharp, radiating pain in the RUQ. Dull pain, on the other hand, tends to be more chronic and less severe, often associated with conditions like irritable bowel syndrome or chronic gastritis – a persistent, uncomfortable ache in the stomach. Cramping pain, often rhythmic and wave-like, is typical of intestinal disorders like constipation or gastroenteritis. The twisting, colicky pain of intestinal gas is a familiar example. Burning pain is frequently indicative of acid reflux or peptic ulcers, a sensation of intense heat in the upper abdomen.
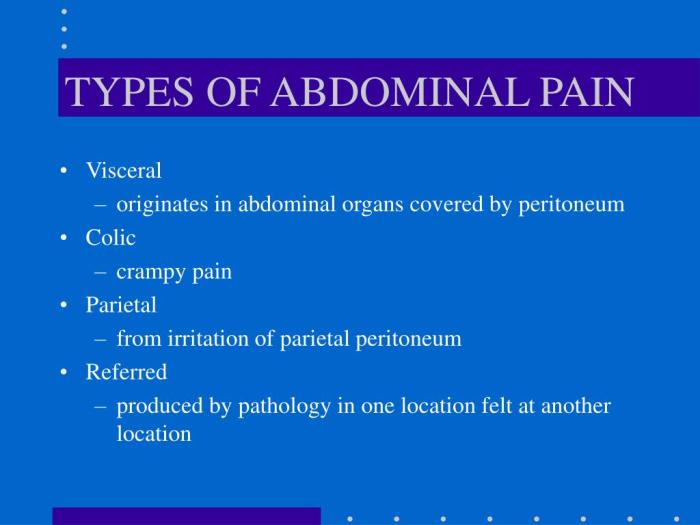
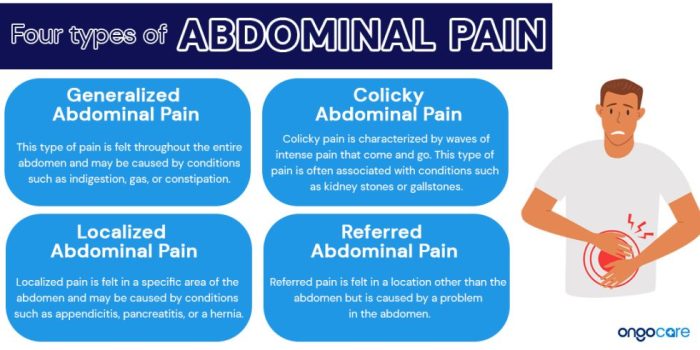
Visceral Versus Somatic Abdominal Pain
Abdominal pain can be broadly categorized into visceral and somatic pain, differing significantly in their origin and presentation. Understanding this distinction is crucial for accurate diagnosis.
| Feature | Visceral Pain | Somatic Pain |
|---|---|---|
| Origin | Stretching or distension of organs; inflammation or ischemia of visceral structures | Parietal peritoneum (lining of the abdominal cavity); irritation of nerve endings in the abdominal wall |
| Quality | Diffuse, crampy, aching, poorly localized | Sharp, well-localized, intense |
| Location | Difficult to pinpoint; often referred to other areas | Precisely located; usually over the affected organ |
| Aggravating Factors | Organ-specific; e.g., eating for gastritis, bowel movements for diverticulitis | Movement, coughing, deep breathing |
| Examples | Early appendicitis, intestinal obstruction | Peritonitis, appendiceal abscess |
Diagnosing Specific Types of Abdominal Pain
Abdominal pain is a common complaint, encompassing a wide spectrum of potential causes. Accurate diagnosis requires a careful consideration of the pain’s location, character, and associated symptoms, along with a thorough medical history and physical examination. This section focuses on diagnosing abdominal pain stemming from gastrointestinal issues, detailing common conditions, diagnostic approaches, and differentiating features.
Gastrointestinal Conditions Causing Abdominal Pain
Understanding the symptoms and diagnostic approaches for common gastrointestinal conditions is crucial for accurate diagnosis and effective treatment. Several conditions present with abdominal pain, and differentiating between them requires careful observation and testing.
- Appendicitis: Characterized by pain typically starting around the navel, then migrating to the lower right abdomen. Other symptoms include nausea, vomiting, fever, loss of appetite, and tenderness to the touch in the lower right quadrant.
- Gastroenteritis: Often presents with diffuse abdominal cramping, nausea, vomiting, diarrhea, and sometimes fever. The pain is usually less localized than in appendicitis.
- Irritable Bowel Syndrome (IBS): Manifests as recurrent abdominal pain or discomfort, often relieved by defecation, associated with changes in bowel habits (diarrhea, constipation, or both). Other symptoms can include bloating, gas, and mucus in the stool. The pain is often diffuse and cramping.
Diagnostic Tests for Gastrointestinal Issues
Various diagnostic tests aid in identifying the underlying cause of gastrointestinal abdominal pain. The choice of test depends on the suspected condition and the patient’s clinical presentation.
| Test Name | Description | What it Identifies |
|---|---|---|
| Complete Blood Count (CBC) | Measures various components of the blood, including white blood cells. | Infection (elevated white blood cell count in appendicitis or gastroenteritis) |
| Stool Analysis | Examines stool for blood, parasites, bacteria, and other abnormalities. | Infections, inflammatory bowel disease, and other gastrointestinal disorders. |
| Imaging Studies (X-ray, CT scan, Ultrasound) | Visualizes internal organs to detect abnormalities. | Appendiceal inflammation (appendicitis), bowel obstruction, tumors, and other structural issues. |
| Blood Tests (e.g., Inflammatory Markers) | Measures levels of inflammatory markers in the blood. | Inflammation associated with conditions like appendicitis or inflammatory bowel disease. |
Differential Diagnosis of Gastrointestinal Abdominal Pain
Differentiating between various gastrointestinal causes of abdominal pain requires a systematic approach. The following flowchart Artikels a possible diagnostic pathway.
A simplified approach involves considering the location and character of the pain, associated symptoms, and the results of initial investigations. For instance, localized right lower quadrant pain with fever and tenderness strongly suggests appendicitis, while diffuse cramping pain with diarrhea may point towards gastroenteritis. IBS is typically characterized by recurrent pain and altered bowel habits, often without clear inflammatory markers.
Flowchart (Text Representation):
Start –> Abdominal Pain?
Yes –> Location of Pain? (Diffuse/Localized)
Diffuse –> Associated Symptoms? (Diarrhea/Constipation/Bloating) –> Consider Gastroenteritis or IBS (Further investigation needed to differentiate)
Localized –> Location? (Right Lower Quadrant/Other)
Right Lower Quadrant –> Fever/Tenderness? –> Consider Appendicitis (Immediate medical attention needed)
Other –> Consider other causes (e.g., bowel obstruction, kidney stones) (Further investigation needed)
No –> Investigate other causes of abdominal discomfort.
Diagnosing Specific Types of Abdominal Pain
Abdominal pain can stem from a wide variety of sources beyond the gastrointestinal tract. Understanding the nuances of pain associated with genitourinary and other systemic conditions is crucial for accurate diagnosis and effective management. This section will explore the characteristics of abdominal pain related to urinary tract infections, kidney stones, liver disease, and pancreatitis, emphasizing the importance of a thorough patient history.
Abdominal Pain Associated with Genitourinary Conditions
Urinary tract infections (UTIs), kidney stones, and other genitourinary issues frequently present with abdominal pain, often localized to the lower abdomen or flanks. Differentiating these conditions requires careful attention to symptom presentation.
UTIs typically cause suprapubic pain (pain above the pubic bone), accompanied by urinary urgency, frequency, burning during urination (dysuria), and potentially cloudy or foul-smelling urine. The pain may be constant or intermittent and can range from mild discomfort to severe cramping. Kidney infections (pyelonephritis), a more severe form of UTI, can cause flank pain (pain in the side, below the ribs), fever, chills, and nausea.
Kidney stones, on the other hand, often present with intense, colicky pain that radiates from the flank to the groin. This pain is often described as excruciating and wave-like, with periods of intense pain followed by relative relief. Nausea, vomiting, and hematuria (blood in the urine) are common accompanying symptoms. Other genitourinary conditions, such as prostatitis (inflammation of the prostate gland) or endometriosis (growth of uterine tissue outside the uterus), may also manifest with abdominal or pelvic pain, often accompanied by other specific symptoms related to the affected organ.
Abdominal Pain Associated with Liver and Pancreatic Disease
Liver and pancreatic diseases can also cause abdominal pain, often with distinct characteristics. These conditions frequently require advanced imaging techniques and laboratory testing for definitive diagnosis.
Liver disease, such as cirrhosis or hepatitis, may cause right upper quadrant pain, often dull and aching. Jaundice (yellowing of the skin and eyes), dark urine, and light-colored stools are common accompanying symptoms. Pancreatitis, an inflammation of the pancreas, typically presents with severe, deep epigastric pain (pain in the upper abdomen) that may radiate to the back. This pain is often accompanied by nausea, vomiting, and fever. The severity of the pain can vary greatly depending on the cause and extent of the inflammation.
Creating a Patient History Focused on Abdominal Pain
A comprehensive patient history is essential for diagnosing abdominal pain. This involves systematically gathering information about the onset, location, duration, character, and associated symptoms of the pain. This structured approach helps narrow down the differential diagnosis.
The following questions are examples and may need modification based on the individual patient’s presentation:
| Aspect of History | Example Questions |
|---|---|
| Onset | When did the pain begin? Was it sudden or gradual? Was it associated with a specific event (e.g., meal, injury)? |
| Location | Where is the pain located? Can you point to it? Does the pain radiate anywhere else? |
| Duration | How long has the pain lasted? Is it constant or intermittent? |
| Character | How would you describe the pain? (e.g., sharp, dull, cramping, burning, stabbing) |
| Associated Symptoms | Do you have any other symptoms, such as nausea, vomiting, fever, diarrhea, constipation, changes in urination, jaundice, or blood in your urine or stool? |
Closing Summary
Mastering the art of diagnosing abdominal pain involves careful consideration of the patient’s history, a thorough physical examination, and the strategic use of diagnostic tests. While this guide provides valuable insights into common causes and diagnostic approaches, it is crucial to remember that self-diagnosis should never replace professional medical advice. The information presented here serves as an educational resource to enhance your understanding and empower you to engage in informed conversations with your healthcare provider. Remember, prompt medical attention is essential for accurate diagnosis and effective treatment of abdominal pain, ensuring optimal health outcomes.