Foot pain can significantly impact daily life, hindering mobility and overall well-being. Understanding the causes of common foot problems is crucial for effective treatment and prevention. This exploration delves into three prevalent conditions: plantar fasciitis, bunions, and ingrown toenails, examining their causes, symptoms, and various treatment approaches. We’ll uncover the intricacies of each condition, providing insights into diagnosis and management strategies to empower individuals in their pursuit of foot health.
Through detailed descriptions of symptoms, diagnostic techniques, and treatment options, this guide aims to equip readers with the knowledge to recognize these conditions and seek appropriate medical attention. We’ll explore both conservative and surgical interventions, emphasizing the importance of early diagnosis and proactive self-care to improve outcomes and prevent complications.
Plantar Fasciitis

Plantar fasciitis is a common cause of heel pain, affecting a significant portion of the population at some point in their lives. Understanding the anatomy involved, common symptoms, and effective treatment strategies is crucial for effective management.
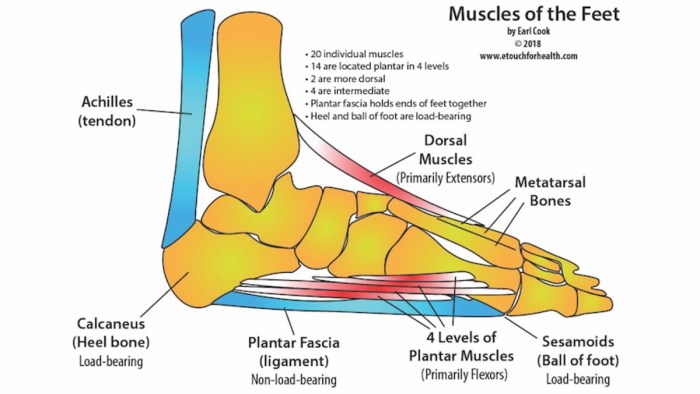
Anatomical Structures Involved in Plantar Fasciitis
Plantar fasciitis primarily involves the plantar fascia, a thick band of tissue on the bottom of the foot that runs from the heel bone (calcaneus) to the toes. This fascia acts as a strong support structure, helping to maintain the arch of the foot and absorb shock during activities like walking and running. Inflammation of this fascia, often due to overuse, strain, or improper footwear, leads to the characteristic pain associated with plantar fasciitis. The pain is often felt most intensely in the heel, but can radiate along the arch of the foot. The calcaneal spur, a bony outgrowth on the heel bone, is sometimes associated with plantar fasciitis, but it’s important to note that the spur itself doesn’t directly cause the pain; rather, it may be a consequence of the chronic inflammation.
Common Symptoms of Plantar Fasciitis
Individuals with plantar fasciitis typically experience heel pain, particularly in the morning or after periods of rest. The pain often worsens with activity and may lessen as the day progresses. Other symptoms can include stiffness in the heel, tenderness to the touch along the plantar fascia, and pain radiating along the arch of the foot. In some cases, plantar fasciitis can also lead to limited range of motion in the ankle and foot. The intensity of symptoms varies greatly among individuals.
Differential Diagnosis of Plantar Fasciitis
Distinguishing plantar fasciitis from other foot conditions is essential for appropriate treatment. Conditions such as heel spurs, Achilles tendinitis, stress fractures, nerve entrapment (such as tarsal tunnel syndrome), and rheumatoid arthritis can present with similar symptoms. A thorough physical examination, including assessment of range of motion, palpation of the affected area, and evaluation of gait, is crucial. Imaging studies, such as X-rays, may be necessary to rule out stress fractures or other bony abnormalities. A detailed medical history, including the onset and progression of symptoms, helps to refine the diagnosis.
Creating a Visual Aid Comparing Treatment Options for Plantar Fasciitis
A table can effectively compare different treatment options for plantar fasciitis. The table should include four columns: Symptom, Severity, Treatment, and Outcome. Here’s a step-by-step guide:
1. Define Symptoms: List common symptoms such as heel pain, arch pain, stiffness, and limited range of motion.
2. Categorize Severity: Use a scale (e.g., mild, moderate, severe) to classify symptom intensity.
3. List Treatments: Include options such as rest, ice, stretching exercises, orthotics, physical therapy, medication (NSAIDs), corticosteroid injections, and surgery (in rare cases).
4. Describe Outcomes: Detail the expected outcomes for each treatment, such as pain reduction, improved mobility, and return to activity.
| Symptom | Severity | Treatment | Outcome |
|---|---|---|---|
| Heel pain | Mild | Rest, ice, stretching | Pain reduction within a few weeks |
| Arch pain, stiffness | Moderate | Orthotics, physical therapy | Improved mobility, reduced pain within several months |
| Severe heel pain, limited mobility | Severe | Corticosteroid injection, surgery (rare) | Significant pain relief, improved function, potential for long-term recovery |
Patient Education Handout: Self-Management Strategies for Plantar Fasciitis
Effective self-management plays a crucial role in managing plantar fasciitis. This handout provides key strategies:
* Rest: Avoid activities that aggravate your pain.
* Ice: Apply ice packs to your heel for 15-20 minutes at a time, several times a day.
* Stretching: Perform regular plantar fascia stretches, such as toe curls and calf stretches. (Detailed instructions should be provided with accompanying illustrations)
* Proper Footwear: Wear supportive shoes with good arch support and cushioning. Avoid high heels or flat, unsupportive footwear.
* Weight Management: If overweight or obese, losing weight can reduce stress on the plantar fascia.
* Over-the-Counter Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce pain and inflammation. Always follow the dosage instructions.
* Orthotics: Custom or over-the-counter arch supports can help improve foot mechanics and reduce stress on the plantar fascia.
Bunions
Bunions, or hallux valgus, are bony bumps that form on the joint at the base of the big toe. This deformity causes the big toe to angle towards the other toes, often resulting in pain, inflammation, and limited mobility. Understanding the factors contributing to bunion development and the available diagnostic and treatment options is crucial for effective management.
Bunion Development Across Age Groups and Genders
Bunions are more prevalent in women than men, likely due to a combination of factors including footwear choices and anatomical differences. While they can develop at any age, they are more common in middle-aged and older adults, often progressing gradually over time. In younger individuals, bunions may be associated with underlying biomechanical issues or inherited predispositions. Older individuals may experience a more rapid progression due to age-related changes in joint cartilage and ligaments. The severity and symptoms can vary significantly between individuals, even within the same age and gender group.
Biomechanical Factors Contributing to Bunion Formation
Several biomechanical factors contribute to bunion formation. These include foot structure (e.g., flat feet, high arches), footwear (e.g., narrow-toed shoes, high heels), and repetitive strain on the big toe joint. Abnormal foot mechanics, such as overpronation (the inward rolling of the foot during walking), can increase stress on the big toe joint, leading to the gradual development of a bunion. The constant pressure from ill-fitting footwear further exacerbates this process, pushing the big toe inwards and causing the bony prominence to enlarge. Genetic predisposition also plays a significant role; individuals with a family history of bunions are at increased risk.
Imaging Techniques for Bunion Diagnosis
Several imaging techniques are used to diagnose bunions and assess their severity. X-rays are the most common method, providing clear images of the bone structure and allowing measurement of the angle of the big toe joint (hallux valgus angle). This helps determine the severity of the deformity. While X-rays are readily available and relatively inexpensive, they don’t show soft tissue structures like ligaments and tendons. Other imaging techniques, such as ultrasound and MRI, can provide more detailed information about the soft tissues but are less commonly used for routine bunion diagnosis due to higher cost and less accessibility. The choice of imaging technique depends on the clinical presentation and the need for detailed information about the soft tissues.
Case Study: Bunion Progression and Treatment
The following table illustrates the progression of a bunion in a 45-year-old female patient:
| Date | Symptoms | Treatment | Outcome |
|---|---|---|---|
| January 2022 | Mild pain and swelling at the base of the big toe; slight redness | Custom orthotics, pain medication | Pain reduced, but swelling persisted |
| July 2022 | Increased pain, swelling, and stiffness; difficulty wearing shoes | Physical therapy, corticosteroid injection | Temporary pain relief, but symptoms recurred |
| January 2023 | Severe pain, significant deformity, limited mobility | Bunionectomy surgery | Significant improvement in pain and mobility; improved cosmetic appearance |
Decision-Making Process for Bunion Management
The decision to pursue conservative or surgical management for bunions depends on several factors, including the severity of the deformity, the level of pain and disability, and the patient’s overall health and preferences. A flowchart can help illustrate this process:
Ingrown Toenails

Ingrown toenails, a common and often painful condition, occur when the edge of a toenail grows into the surrounding skin. This can lead to inflammation, infection, and significant discomfort. Understanding the risk factors, recognizing the symptoms, and knowing the available treatment options are crucial for effective management.
Risk Factors for Ingrown Toenails
Improper toenail trimming is a primary culprit in the development of ingrown toenails. Other factors, such as the type of footwear worn and individual hygiene practices, also play a significant role. Tight-fitting shoes, particularly those with pointed toes, constantly compress the toenails, increasing the likelihood of ingrowth. Poor hygiene, allowing dirt and debris to accumulate under the nail, can exacerbate the problem and lead to infection.
Clinical Presentation of Ingrown Toenails
An ingrown toenail typically presents with pain, redness, and swelling at the affected nail edge, usually the big toe. The skin surrounding the nail may become inflamed and tender to the touch. In more severe cases, pus or other drainage may be present, indicating an infection. The nail itself may appear deformed or partially embedded in the skin. Individuals may also experience throbbing pain, especially when wearing shoes.
Treatment Methods for Ingrown Toenails
The following table compares different treatment methods for ingrown toenails, ranging from conservative approaches to surgical intervention.
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Conservative Management | Soaking the foot in warm, soapy water, applying antibiotic ointment, and keeping the area clean and dry. This may include using cotton or dental floss to gently lift the ingrown nail edge. | Non-invasive, relatively inexpensive, often effective for mild cases. | May not be effective for severe infections or recurrent ingrown toenails; can be time-consuming. |
| Partial Nail Avulsion | Surgical removal of a portion of the ingrown nail. A local anesthetic is typically used. | Effective for moderate to severe ingrown toenails; reduces recurrence rate compared to conservative management. | Requires a surgical procedure; carries a small risk of complications such as bleeding or infection. |
| Complete Nail Avulsion | Surgical removal of the entire toenail. This is usually reserved for severe or recurrent cases. | Highly effective for severe or recurrent ingrown toenails. | More invasive than partial avulsion; carries a higher risk of complications; may result in a longer healing period. |
| Phenol Matrixectomy | Chemical destruction of the nail matrix (the area where the nail grows from) to prevent regrowth of the ingrown portion of the nail. | Effective in preventing recurrence; often combined with partial or complete avulsion. | May cause temporary or permanent nail deformity; requires expertise. |
Nail Avulsion Technique
Nail avulsion, the surgical removal of the nail, should only be performed by a qualified medical professional. The procedure typically involves the following steps: First, the area is thoroughly cleaned and anesthetized. Then, a small incision is made to separate the ingrown nail from the surrounding skin. The nail is carefully lifted and removed using specialized instruments. The wound is then cleaned and dressed. Post-operative care instructions, including keeping the area clean and dry, are provided to the patient. Antibiotics may be prescribed to prevent infection.
Patient Education on Toenail Trimming
Proper toenail trimming is essential for preventing ingrown toenails. Here are some key points to emphasize to patients:
The following instructions are crucial for preventing ingrown toenails. Adherence to these guidelines can significantly reduce the risk of this common and painful condition.
- Trim toenails straight across, avoiding rounding the corners.
- Use sharp nail clippers to ensure a clean cut.
- Avoid trimming toenails too short.
- Keep toenails clean and dry.
- Wear properly fitting shoes that do not compress the toenails.
Concluding Remarks
Successfully navigating foot problems requires a comprehensive understanding of their underlying causes and effective management strategies. By recognizing the distinct characteristics of plantar fasciitis, bunions, and ingrown toenails, individuals can take proactive steps towards alleviating pain and restoring foot health. Remember, early diagnosis and appropriate treatment are key to minimizing discomfort and preventing long-term complications. This guide serves as a valuable resource for individuals seeking to understand and manage these common foot ailments, empowering them to make informed decisions about their care.