Experiencing low blood sugar, or hypoglycemia, can be unsettling. Understanding its various causes is crucial for effective management and prevention. This guide explores seven common culprits behind low blood sugar, detailing their physiological mechanisms, associated symptoms, and diagnostic approaches. We’ll also delve into strategies for managing and preventing future episodes, empowering you to take control of your health.
From the intricacies of insulin regulation to the impact of dietary choices, we’ll unravel the complexities of hypoglycemia. We’ll cover diagnostic tests like blood glucose measurements and continuous glucose monitoring (CGM), helping you understand how to interpret results and work with your healthcare provider to develop a personalized management plan. This comprehensive guide aims to equip you with the knowledge to navigate the challenges of low blood sugar and live a healthier life.
Common Causes of Low Blood Sugar (Hypoglycemia)
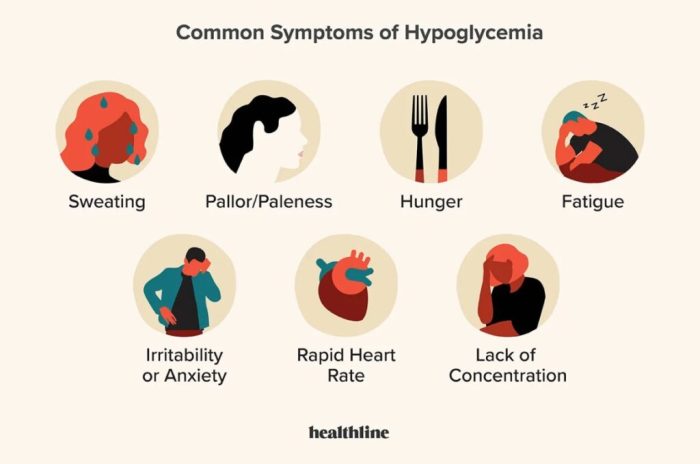
Hypoglycemia, or low blood sugar, occurs when your blood glucose levels drop below the normal range. This can be caused by a variety of factors, ranging from medication side effects to underlying medical conditions. Understanding the common causes, their associated symptoms, and potential triggers is crucial for effective management and prevention.
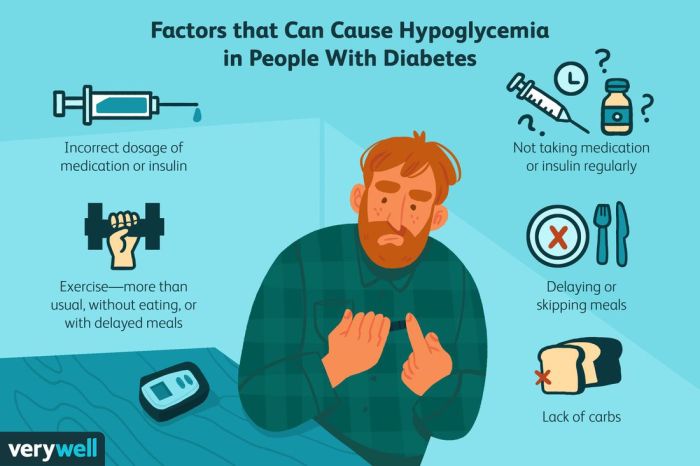
Insulin Overdose or Improper Timing
Insulin, a hormone that helps glucose enter cells, is essential for managing blood sugar in people with diabetes. An overdose of insulin, or taking insulin too close to a meal or without sufficient carbohydrate intake, can lead to a significant drop in blood glucose. Symptoms can range from mild shakiness and sweating to confusion, seizures, and loss of consciousness. The onset is typically rapid, often within hours of insulin administration. Lifestyle factors like inconsistent meal timing, skipping meals, or intense physical activity without adjusting insulin dosage can exacerbate this cause.
Reactive Hypoglycemia
This type of hypoglycemia occurs after eating a meal high in simple carbohydrates. The rapid rise and subsequent fall in blood sugar levels trigger an overreaction from the pancreas, releasing excessive insulin. Symptoms include dizziness, lightheadedness, anxiety, and sweating, usually appearing within 2-4 hours after a meal. Frequent consumption of sugary drinks and refined carbohydrates are significant lifestyle factors that contribute to reactive hypoglycemia.
Alcohol Consumption
Alcohol interferes with the liver’s ability to produce glucose, leading to a drop in blood sugar levels. This effect is amplified when alcohol is consumed on an empty stomach. Symptoms can include confusion, slurred speech, incoordination, and even unconsciousness. The onset can be gradual, but symptoms often become more pronounced several hours after drinking. Binge drinking and consuming alcohol without food are key lifestyle factors that increase the risk.
Insufficient Food Intake
Prolonged fasting, skipping meals, or consuming insufficient calories can lead to low blood sugar, particularly in individuals with diabetes or those taking certain medications. Symptoms are generally gradual in onset, starting with fatigue, weakness, and irritability, and potentially progressing to more severe symptoms if untreated. Irregular eating patterns and restrictive diets are prominent lifestyle factors.
Certain Medications
Several medications, including some insulin secretagogues (used to treat type 2 diabetes), beta-blockers (used to treat high blood pressure), and salicylates (aspirin), can contribute to hypoglycemia. The mechanism varies depending on the medication but often involves increased insulin secretion or impaired glucose production. Symptoms mirror those of other causes and onset depends on the medication’s pharmacokinetics. Over-reliance on medication without proper dietary management can exacerbate this cause.
Hormonal Disorders
Conditions like adrenal insufficiency (Addison’s disease) and hypopituitarism can affect hormone production, leading to impaired glucose regulation and hypoglycemia. Symptoms vary depending on the underlying hormonal imbalance but often include fatigue, weakness, and weight loss. The onset is typically gradual. Stress and inadequate management of the underlying hormonal disorder are key lifestyle factors.
Rare Inherited Metabolic Disorders
Certain rare genetic disorders affect the body’s ability to process glucose effectively, leading to hypoglycemia. These conditions often manifest in infancy or childhood. Symptoms can be varied and severe, including seizures, developmental delays, and organ dysfunction. The onset is typically early in life and is largely influenced by genetic predisposition.
Comparison of Common Causes of Hypoglycemia
| Cause | Symptoms | Common Risk Factors | Potential Complications |
|---|---|---|---|
| Insulin Overdose/Improper Timing | Shakiness, sweating, confusion, seizures, loss of consciousness | Diabetes, inconsistent meal timing, intense exercise without insulin adjustment | Seizures, coma, death |
| Reactive Hypoglycemia | Dizziness, lightheadedness, anxiety, sweating | High simple carbohydrate intake, rapid blood sugar fluctuations | Falls, impaired cognitive function |
| Alcohol Consumption | Confusion, slurred speech, incoordination, unconsciousness | Alcohol abuse, drinking on an empty stomach | Severe hypoglycemia, accidents, coma |
| Insufficient Food Intake | Fatigue, weakness, irritability, dizziness | Skipping meals, restrictive diets, prolonged fasting | Severe hypoglycemia, impaired cognitive function |
| Certain Medications | Variable, often similar to other causes | Use of insulin secretagogues, beta-blockers, salicylates | Severe hypoglycemia, organ damage |
| Hormonal Disorders (e.g., Addison’s disease) | Fatigue, weakness, weight loss, low blood pressure | Adrenal insufficiency, hypopituitarism | Severe hypoglycemia, organ damage, death |
| Inherited Metabolic Disorders | Variable, often severe and including seizures, developmental delays | Genetic predisposition | Severe hypoglycemia, organ damage, developmental delays, death |
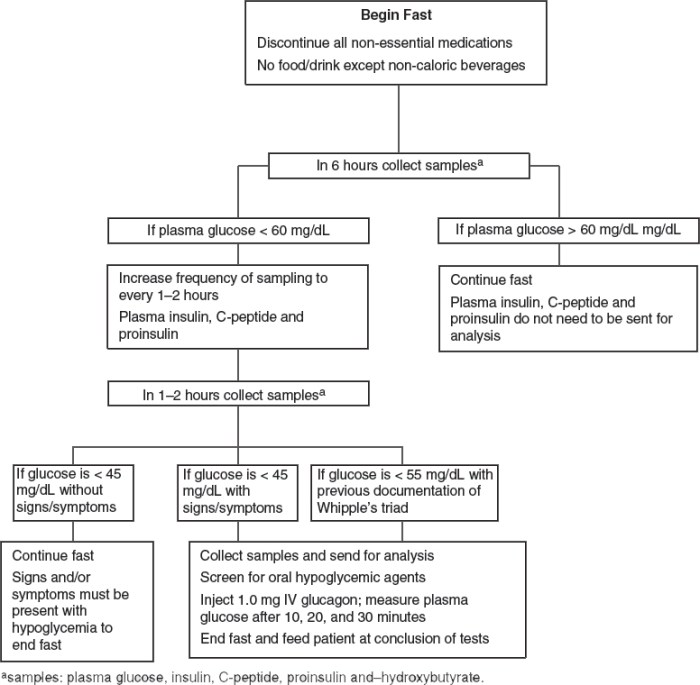
Diagnostic Procedures for Low Blood Sugar
Diagnosing low blood sugar, or hypoglycemia, involves a combination of blood tests and potentially other investigations to pinpoint the underlying cause. Accurate diagnosis relies on careful measurement of blood glucose levels at specific times and in relation to symptoms. The process helps differentiate between reactive hypoglycemia (occurring after meals) and fasting hypoglycemia (occurring while fasting).
Blood Glucose Testing
Blood glucose testing is the cornerstone of hypoglycemia diagnosis. This involves measuring the concentration of glucose in a blood sample. There are two primary methods: fasting blood glucose tests and random blood glucose tests. A fasting blood glucose test requires abstaining from food and drink (except water) for at least 8 hours before the test. This allows for accurate assessment of baseline glucose levels. A random blood glucose test can be performed at any time, regardless of food intake, and is useful for assessing glucose levels when symptoms occur. The results are interpreted in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Normal fasting blood glucose levels generally range from 70 to 100 mg/dL (3.9 to 5.6 mmol/L), while values below 70 mg/dL (3.9 mmol/L) may indicate hypoglycemia. However, interpretation must consider the individual’s medical history, medication use, and the timing of the test relative to meals. A low random blood glucose level alongside hypoglycemic symptoms is significant, even if the fasting level is within the normal range.
Interpreting Blood Glucose Levels
Interpreting blood glucose levels requires considering several factors. The time of day influences glucose levels; they are typically lowest in the early morning hours before breakfast. Recent food intake significantly impacts glucose levels; a postprandial (after-meal) blood glucose test is crucial in diagnosing reactive hypoglycemia. The presence of symptoms, such as sweating, shakiness, confusion, or fainting, alongside low blood glucose readings is essential for a definitive diagnosis. A single low blood glucose reading might not be diagnostic; several measurements taken at different times, particularly when symptoms are present, are often necessary. For instance, a person experiencing symptoms of hypoglycemia might have a blood glucose level of 50 mg/dL (2.8 mmol/L) one hour after a meal, even if their fasting blood glucose is normal.
Continuous Glucose Monitors (CGMs)
Continuous glucose monitors (CGMs) provide continuous glucose readings throughout the day and night. These devices offer a more comprehensive picture of glucose fluctuations than intermittent finger-stick testing. CGMs are particularly valuable in diagnosing and managing hypoglycemia, as they can detect both frequent and subtle episodes of low blood glucose that might be missed with traditional testing. This continuous monitoring allows for identification of patterns and triggers of hypoglycemia, which is essential for personalized management strategies. For example, a CGM might reveal a pattern of hypoglycemia occurring consistently two hours after dinner, suggesting a need for dietary adjustments.
Additional Diagnostic Tests
To determine the underlying cause of hypoglycemia, additional tests may be necessary. These tests aim to identify potential problems with insulin production, hormone imbalances, or other medical conditions.
- Insulin Tests: Measuring insulin levels in the blood during a hypoglycemic episode can help determine whether excessive insulin production is contributing to low blood glucose.
- C-peptide levels: Measuring C-peptide, a byproduct of insulin production, helps differentiate between endogenous (body’s own) and exogenous (externally administered) insulin as the cause of hypoglycemia.
- Hormone Level Checks: Assessing levels of hormones like cortisol, glucagon, and growth hormone can identify hormonal imbalances that might be contributing to hypoglycemia.
- Liver Function Tests: Evaluating liver function is important as the liver plays a crucial role in glucose metabolism.
- Genetic testing: In some cases, genetic testing may be considered to identify inherited conditions that affect glucose metabolism.
Managing and Preventing Low Blood Sugar
Managing and preventing low blood sugar, or hypoglycemia, requires a multifaceted approach tailored to the individual’s specific needs and underlying causes. Effective strategies involve careful monitoring, dietary adjustments, medication management, and lifestyle changes to maintain stable blood glucose levels. This section details effective methods for managing and preventing hypoglycemic episodes.
Dietary Adjustments for Hypoglycemia Management
Dietary adjustments are crucial in managing hypoglycemia. Individuals should focus on consuming regular, balanced meals and snacks throughout the day to prevent blood sugar from dropping too low. These meals and snacks should include a combination of complex carbohydrates, protein, and healthy fats. Complex carbohydrates, such as whole grains, fruits, and vegetables, provide sustained energy release, preventing rapid spikes and crashes in blood sugar. Protein and healthy fats help slow down the absorption of carbohydrates, further stabilizing blood glucose levels. For example, a snack combining a small apple with a handful of almonds provides both carbohydrates and healthy fats for sustained energy. Portion control is also vital; consuming excessively large amounts of carbohydrates can lead to postprandial (after-meal) hypoglycemia in some individuals. Working with a registered dietitian or certified diabetes educator can help create a personalized meal plan.
Medication Management for Hypoglycemia
Medication management is essential for individuals with diabetes or other conditions that predispose them to hypoglycemia. This may involve adjusting the dosage or timing of medications, such as insulin or oral hypoglycemic agents, under the close supervision of a physician. For example, individuals using insulin may need to adjust their insulin dose based on their activity level, food intake, and blood glucose monitoring results. Regular communication with healthcare providers is critical to ensure the medication regimen effectively manages blood sugar without causing hypoglycemic episodes. Careful monitoring of blood glucose levels, using a glucose meter, allows for proactive adjustments to medication and dietary intake as needed.
Lifestyle Changes to Prevent Hypoglycemia
Lifestyle changes play a significant role in preventing hypoglycemia. Regular physical activity helps improve insulin sensitivity, reducing the risk of low blood sugar. However, it’s important to avoid exercising during periods of low blood sugar. Adequate sleep is also crucial; lack of sleep can negatively impact blood sugar control. Stress management techniques, such as yoga or meditation, can also help regulate blood glucose levels. Maintaining a healthy weight through a balanced diet and regular exercise can significantly contribute to better blood sugar control and reduce the risk of hypoglycemia. Consistent adherence to these lifestyle modifications can significantly reduce the frequency and severity of hypoglycemic episodes.
Creating a Personalized Hypoglycemia Management Plan
A personalized hypoglycemia management plan should be developed in collaboration with a healthcare provider, taking into account individual factors such as age, overall health, medications, and lifestyle. This plan should include specific guidelines on meal timing, carbohydrate intake, medication adjustments, and strategies for managing hypoglycemic episodes. Regular monitoring of blood glucose levels is crucial for tracking effectiveness and making necessary adjustments to the plan. The plan should also Artikel strategies for managing stress and incorporating regular physical activity. Regular follow-up appointments with the healthcare provider are essential to monitor progress, address any concerns, and make necessary modifications to the plan as needed. This collaborative approach ensures the plan is both effective and sustainable.
Emergency Treatment for Severe Hypoglycemia
Severe hypoglycemia is a medical emergency requiring immediate treatment. The following steps Artikel emergency procedures for severe hypoglycemia, and this information should be included in any patient handbook.
| Step | Action |
|---|---|
| 1 | Check blood glucose level immediately using a glucose meter. |
| 2 | If blood glucose is dangerously low (generally below 70 mg/dL), administer a fast-acting source of sugar. This could include 15-20 grams of glucose in the form of glucose tablets, gel, or 4 ounces of juice or regular soda. |
| 3 | Recheck blood glucose level after 15 minutes. If still low, repeat step 2. |
| 4 | If symptoms do not improve or if the individual is unconscious or unable to swallow, immediately call emergency medical services (911 or your local emergency number). |
| 5 | Once blood glucose is stable, consume a complex carbohydrate and protein-containing snack or meal to prevent further episodes. |
Always carry a fast-acting sugar source and inform family and friends about the signs and symptoms of hypoglycemia and how to provide assistance.
End of Discussion
Successfully managing hypoglycemia requires a multifaceted approach encompassing understanding its causes, employing appropriate diagnostic tools, and implementing effective management strategies. By recognizing the symptoms, identifying potential triggers, and working closely with your healthcare provider, you can significantly reduce the frequency and severity of low blood sugar episodes. Remember, proactive management, including dietary adjustments, medication adherence (if applicable), and regular monitoring, is key to maintaining stable blood glucose levels and overall well-being.