Understanding pain is crucial for effective treatment. This guide delves into the diagnosis of ten common pain types, exploring their unique characteristics and diagnostic pathways. We’ll examine both the subjective experience of pain and the objective findings from physical examinations and imaging studies, providing a comprehensive approach to identifying the root cause of your discomfort.
From the sharp sting of a nerve injury to the dull ache of muscle strain, pain manifests in diverse ways. We’ll navigate the complexities of differentiating between these varied presentations, outlining diagnostic methods tailored to each pain type. This detailed exploration will equip you with a clearer understanding of how healthcare professionals approach pain diagnosis and the importance of seeking professional medical advice for persistent or severe pain.
Understanding Pain Types
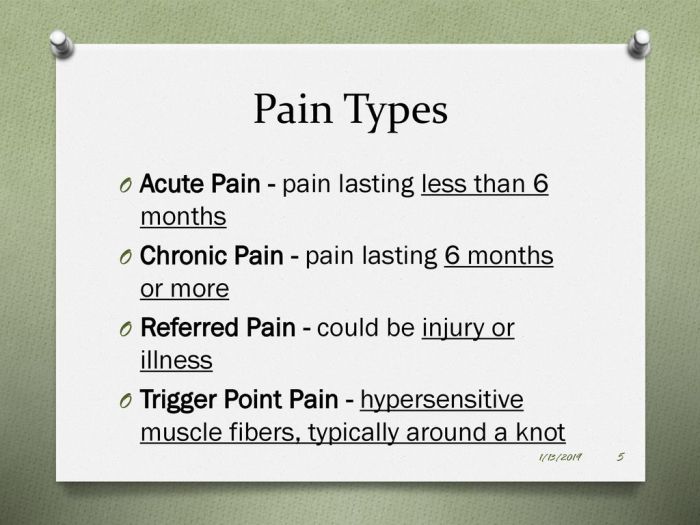
Pain is a complex experience, varying widely in its nature, location, and intensity. Understanding the different types of pain is crucial for effective diagnosis and treatment. This section will explore the fundamental differences between neuropathic and nociceptive pain, followed by detailed descriptions of ten common pain types.
Nociceptive vs. Neuropathic Pain
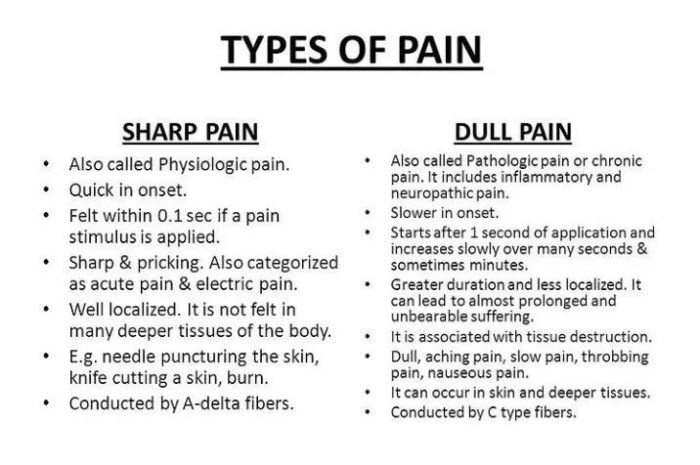
Nociceptive pain arises from the activation of nociceptors, specialized nerve endings that detect noxious stimuli like heat, cold, pressure, or chemicals released during tissue damage. It’s typically sharp, localized, and serves as a warning signal of potential injury. Neuropathic pain, on the other hand, originates from damage or dysfunction within the nervous system itself. This can involve nerves in the peripheral or central nervous system. It is often described as burning, tingling, shooting, or stabbing and may be accompanied by numbness or hypersensitivity. The key difference lies in the source: nociceptive pain stems from tissue damage, while neuropathic pain originates from nerve damage.
Ten Types of Pain and Their Characteristics
The following section details ten common types of pain, their causes, manifestations, and key characteristics.
| Pain Type | Location | Intensity | Duration | Quality | Common Causes | Example Manifestation |
|---|---|---|---|---|---|---|
| Somatic Pain | Skin, muscles, bones, joints | Variable; can be mild to severe | Variable; acute or chronic | Aching, throbbing, sharp | Injury, inflammation, overuse | Muscle strain causing aching in the back |
| Visceral Pain | Internal organs | Variable; often severe | Variable; acute or chronic | Cramping, squeezing, pressure | Organ damage, inflammation, distension | Sharp, cramping pain in the abdomen during appendicitis |
| Neuropathic Pain | Along nerve pathways | Variable; often severe | Chronic | Burning, tingling, shooting, stabbing | Nerve damage (diabetes, shingles, injury) | Numbness and tingling in the hands and feet due to diabetic neuropathy |
| Referred Pain | Different location than source | Variable | Variable | Aching, burning, sharp | Internal organ damage radiating to other areas | Heart attack pain radiating to the left arm |
| Inflammatory Pain | Area of inflammation | Variable; often severe | Variable; acute or chronic | Aching, throbbing, sharp | Inflammation (arthritis, injury) | Swelling and pain in a joint due to arthritis |
| Musculoskeletal Pain | Muscles, bones, joints | Variable | Variable | Aching, stiffness, sharp | Injury, overuse, arthritis | Stiff neck after sleeping in an awkward position |
| Headache Pain | Head | Mild to severe | Variable | Throbbing, sharp, dull | Tension, migraine, sinus infection | Throbbing headache on one side of the head (migraine) |
| Facial Pain | Face | Variable | Variable | Sharp, burning, aching | Neuralgia, sinus infection, dental problems | Sharp, shooting pain in the face (trigeminal neuralgia) |
| Phantom Limb Pain | Amputated limb | Variable; often severe | Chronic | Burning, tingling, cramping | Nerve damage after amputation | Pain felt in a missing leg after amputation |
| Central Pain | Brain or spinal cord | Variable; often severe | Chronic | Burning, tingling, shooting | Damage to the central nervous system (stroke, multiple sclerosis) | Burning pain on one side of the body after a stroke |
Diagnostic Methods for Pain
Accurately diagnosing the source of a patient’s pain is crucial for effective treatment. A multifaceted approach, incorporating several diagnostic methods, is typically employed to achieve this. This process combines subjective information gathered from the patient’s description of their pain with objective findings from various examinations and tests.
Physical Examination
A thorough physical examination forms the cornerstone of pain diagnosis. The physician observes the patient’s posture, gait, and range of motion, noting any limitations or abnormalities. Palpation, or feeling the affected area, helps identify tenderness, swelling, muscle spasms, or other physical signs. Specific tests may be performed depending on the suspected source of pain; for example, a musculoskeletal examination might involve assessing joint stability and muscle strength. The physical examination provides valuable clues to the location, nature, and potential cause of the pain.
Imaging Techniques
Imaging techniques offer a non-invasive way to visualize internal structures and identify potential sources of pain. X-rays are useful for detecting fractures, dislocations, and some types of arthritis. Magnetic resonance imaging (MRI) provides detailed images of soft tissues, including muscles, ligaments, tendons, and nerves, making it particularly valuable for diagnosing conditions like herniated discs, muscle tears, and spinal stenosis. Computed tomography (CT) scans produce cross-sectional images, offering excellent visualization of bones and internal organs, and are often used to assess trauma or identify tumors. The choice of imaging technique depends on the suspected cause of the pain and the specific anatomical area involved. For example, an MRI might be chosen to assess back pain, while an X-ray would be more appropriate for suspected fractures in a limb.
Neurological Examination
A neurological examination assesses the function of the nervous system to determine if nerve damage or dysfunction is contributing to the pain. This involves testing reflexes, muscle strength, sensation (touch, temperature, pain), and coordination. Specific tests may be used to evaluate nerve function, such as assessing dermatomes (areas of skin innervated by specific nerves) or testing for nerve root compression. Findings from a neurological examination can help differentiate between musculoskeletal pain and pain arising from nerve compression or other neurological conditions. For example, numbness or tingling in a specific dermatome might indicate nerve root compression, suggesting a potential source of back pain.
Blood Tests
Several blood tests can help identify underlying medical conditions that may be causing or contributing to pain. These tests may include a complete blood count (CBC) to assess for infection or inflammation, inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), and tests to assess for autoimmune diseases or metabolic disorders. Blood tests are not always diagnostic for pain itself but can help rule out other conditions or identify systemic problems that may be contributing to the pain experience. For instance, elevated inflammatory markers might suggest an inflammatory arthritis as the source of joint pain. The results are interpreted in conjunction with the patient’s history and the findings from other diagnostic tests.
Diagnostic Pathway Flowchart
A simplified flowchart illustrating a potential diagnostic pathway:
[Imagine a flowchart here. It would start with “Patient presents with pain,” branching to “Physical Exam,” “Patient History,” and “Initial Assessment.” The “Physical Exam” branch would lead to “Normal Findings” (potentially leading to further investigations like imaging or blood tests) or “Abnormal Findings” (leading directly to a potential diagnosis). The “Patient History” branch would consider factors like location, onset, duration, character of pain, and associated symptoms. The “Initial Assessment” branch would consider the patient’s overall presentation, leading to targeted investigations. The flowchart would converge at a “Diagnosis and Treatment Plan” stage.] The flowchart would demonstrate how different tests and examinations are chosen based on the initial assessment and the information gathered during the patient’s history and physical examination. This iterative process of assessment and testing allows for a more precise diagnosis.
Specific Pain Types and Their Diagnosis

Differentiating between various pain types is crucial for effective treatment. Accurate diagnosis relies on a combination of patient history, physical examination, and sometimes, further investigations like imaging or blood tests. This section will detail the diagnostic approaches for several common pain types, highlighting key differentiating features.
Headache Types: Tension, Migraine, and Cluster
Headaches are a common complaint, but their underlying causes can vary significantly. Differentiating between tension headaches, migraines, and cluster headaches requires careful consideration of the pain’s characteristics, location, and associated symptoms. Tension headaches are typically bilateral, pressing or tightening in quality, and are not worsened by physical activity. Migraines, on the other hand, often present as unilateral, throbbing pain, frequently accompanied by nausea, vomiting, and photophobia or phonophobia. Cluster headaches are characterized by severe, unilateral pain around the eye, often accompanied by tearing, nasal congestion, and facial sweating. Diagnosis is primarily clinical, based on the patient’s description of their symptoms.
Back Pain Diagnosis: Muscular, Nerve-Related, and Structural Causes
Back pain is a prevalent issue with diverse etiologies. Muscular back pain is often characterized by aching, stiffness, and localized tenderness, typically improving with rest and movement. Nerve-related back pain, such as sciatica, involves radiating pain down the leg, often accompanied by numbness, tingling, or weakness. Structural causes, like spinal stenosis or disc herniation, may present with more persistent, severe pain, potentially accompanied by neurological deficits. Diagnosis involves a thorough physical examination, assessing range of motion, neurological function, and palpation for tenderness. Imaging studies, such as X-rays or MRIs, may be necessary to identify structural abnormalities.
Neck and Shoulder Pain Diagnostic Approaches
Neck and shoulder pain often coexist and share similar diagnostic approaches. Neck pain can originate from muscular strain, cervical spondylosis (degenerative changes in the neck), or nerve compression. Shoulder pain can stem from rotator cuff injuries, bursitis, arthritis, or referred pain from the neck or other areas. Diagnosis involves evaluating range of motion, muscle strength, and neurological function. Imaging, such as X-rays or MRIs, may be helpful in identifying structural issues. Careful history-taking, differentiating between acute and chronic pain, and the presence of associated symptoms are crucial for accurate diagnosis.
Diagnosing and Differentiating Abdominal Pain Types
Abdominal pain encompasses a broad spectrum of conditions, ranging from relatively benign to life-threatening. The location, character, and associated symptoms are crucial for diagnosis. For example, appendicitis typically presents with right lower quadrant pain, often starting around the umbilicus and becoming progressively more localized and severe. Gallstones may cause right upper quadrant pain, often radiating to the back. Gastroenteritis usually presents with diffuse abdominal cramping, nausea, vomiting, and diarrhea. A thorough history, physical examination, and potentially blood tests or imaging studies (ultrasound, CT scan) are vital for accurate diagnosis and to rule out serious conditions.
Key Diagnostic Features for Ten Pain Types
The following Artikels key diagnostic features for ten common pain types. Note that this is not exhaustive, and further investigation may be necessary in individual cases.
- Headache (Tension): Bilateral, pressing/tightening, no worsening with activity.
- Headache (Migraine): Unilateral, throbbing, nausea/vomiting/photophobia/phonophobia.
- Headache (Cluster): Severe unilateral pain around the eye, tearing/congestion/sweating.
- Back Pain (Muscular): Aching, stiffness, localized tenderness, improves with rest.
- Back Pain (Nerve-related): Radiating leg pain, numbness/tingling/weakness.
- Back Pain (Structural): Persistent severe pain, potential neurological deficits.
- Neck Pain: Pain in the neck, may radiate to the arm, limited range of motion.
- Shoulder Pain: Pain in the shoulder, limited range of motion, potential weakness.
- Abdominal Pain (Appendicitis): Right lower quadrant pain, often starting periumbilical.
- Abdominal Pain (Gallstones): Right upper quadrant pain, may radiate to the back.
Last Word
Successfully diagnosing pain requires a multi-faceted approach, combining patient history, physical examination, and advanced imaging techniques. By understanding the unique characteristics of different pain types and employing appropriate diagnostic methods, healthcare professionals can pinpoint the underlying cause and develop effective treatment strategies. This guide provides a foundational understanding of this complex process, emphasizing the importance of seeking professional medical advice for accurate diagnosis and personalized care.